Well, Rick, I'm an optimistic guy. Today, however, I'm going to go with my gut instinct and say that the new CDC idea of replacing VAP with VAE is simply B-A-D. I hate to be negative, but that's the general tone I think I must take with this new algorithm. I think it's simply BAD. Anything that is lead by a government agency, which the CDC is, is generally going to be BAD. It's not going to save money, and it will not save lives. All it's going to do is screw somebody, and in this case it's the hospital, and (if they close as a result), the patient.
If you get too complicated, people are simply going to lose interest. A good example is all the side effects and risks associated with medicines. I bet most people don't even bother to read the package inserts anymore, because to do so you'd have to spend hours doing it. So most people take those package inserts and toss them in the trash. How many trees do you think are wasted because of these package inserts? I bet millions. If environmentalists want to save trees, they should get rid of lawyers, because they're the reason for all the package inserts. Getting rid of lawyers, or (hey! I have a good idea) tort reform that prevents them from suing for millions and screwing doctors, would be the best way to reduce healthcare costs. Yet, the government does the opposite, and it creates more regulations. Ah, and it gets even more confusing.
However, I digress. There is another thing that I think is becoming too complicated, and it's the new recommendations to prevent ventilator acquired (or associated) pneumonia (VAP). I think it's great to make efforts at improving patient care, yet the efforts ought to be simple. Currently at our hospital we do this by the following:
- Ventilator Weaning Protocol (get patient off the ventilator as soon as possible)
- Keeping the cuff pressure 20 or higher (studies show it should be 30 or higher) This means no more minimal occluding volume. The idea is the patient should be removed from the vent before. At pressures under 30 some fluids leak to the lungs, causing pneumonia.
- Patients head should be elevated 30 degrees to prevent aspiration.
- Oral cavity should be cleaned about every 2 hours (studies show this cleans the mouth of bacteria that might cause pneumonia.
- Inline suctioning (ballards) should be used in lieu of taking patient off the vent and bagging
A recent article in RT Magazine, "VAE is the New VAP," (an article by Mark Grzeskowiak, RRT )suggests, as the title notes, VAP should be replaced with VAE. I read the article, and I think the VAE is way too complicated. VAE stands for (Ventilator Associated Events). So we're looking at more than just preventing pneumonia, we are now looking at preventing other things that are caused by the ventilator and may cause an increased hospital stay. Nah, the real purpose of this is not to help the patient, it's to create yet another excuse for the government not to have to pay for a patients hospital visit. Since VAP didn't do it, now they're creating VAE in order to make it almost impossible to comply. "Hah!" says Uncle Sam, "Take that!"
So ventilator bundles are working, but, as noted by Grzeskowiak:
If there is an intention to reward those who do a good job of preventing hospital-acquired infections, the objective basis for VAP diagnosis should be sound. Unfortunately, it is not. As an example, the current criteria attempt to quantify VAP with an evaluation of the patient’s sputum. Changes in consistency, color, or quantity were felt to be indicative of a pneumonic process. Unfortunately, these terms are far too subjective to be of any real scientific value. A change in a patient’s chest x-ray is another confirmatory indicator. The presence of a new or persistent infiltrate is considered to be a sign of impending compromise. But the variability in both radiographic technique and the opinions of interpreting radiologists makes this an equally unreliable indicator. In their Ventilator-Associated Event Protocol, the National Health and Safety Network describes the currently used criteria as “neither sensitive nor specific.” If this statement is correct, a number of questions occur. If you cannot reliably confirm VAP, how do you know what your rates really are? Also, how would you know if a prevention strategy is working?So basically something positive is no longer good enough, and the reason is because the government is not saving enough. Since too many patients are no longer getting VAP, the government doesn't have an excuse not to pay. So now we have VAE, which means increased standards, with means a much more complicated definition, and too much to think about. If what we do already is burning us RTs out, consider the new VAE criteria that I will list below (as noted by Grzeskowiak).
According to Grzeskowiak, there will be a "new algorithm that will include definitions for three potentially preventable events that could develop in ventilator patients. Those tiers include 1) ventilator-associated conditions (VAC), 2) infection-related ventilator-associated conditions (IVAC), and 3) possible or probable VAP. One should anticipate seeing the changes in terminology described below.
Ventilator-Associated Events (VAE)
Ventilator-Associated Conditions (VAC)
Infection-Related Ventilator-Associated Conditions (IVAC)
Probable/Possible Ventilator-Associated Pneumonia (VAP)"
The algorithm goes something like this:Ventilator-Associated Conditions (VAC)
Infection-Related Ventilator-Associated Conditions (IVAC)
Probable/Possible Ventilator-Associated Pneumonia (VAP)"
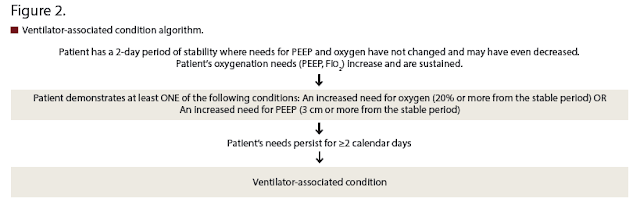
Ventilator Associated Conditions, defined as the patient is not getting better, are also considered part of the algorith. Ventilator Associated Conditions are shown here:
Basically, if the patient's oxygen needs decrease withing the first couple days, and then the patient gets worse and requires more oxygen again, this is a Ventilator Acquired Condition. Since this is part of the government's pay for performance program, if you are not doing an adequate job of limiting VAE, your hospital could be punished. The patient's stay at your hospital may not be reimbursed. Trust me folks, this is yet another attempt by the government to squeeze hospitals out of money, and at the same time giving Uncle Sam an excuse not to pay. Who benefits? No one. Healthcare gets worse, hospitals can't afford to stay independent, so they merge or close their doors.
Thankfully, according to Grzeskowiak: "The CDC states that the algorithm is used for surveillance purposes only and is not intended to guide the clinical management of patients. The guidelines in their entirety can be found at www.cdc.gov and searching for “ventilator-associated event protocol.” But we know what that means: hospital admins will create more order sets, that will make RTs do more. Hospitals will have to fork out more money, and the government will have its excuse not to pay. Yay! Sounds Great to me!
As noted, the views of Will are not necessarily mine. Will has his own independent way of looking at things, and even when I disagree with him I respect that. Please chime in with your thoughts. If you don't respond, then we will assume you agree with Will. Or, perhaps, if nothing else, he gets you to thinking. If so, let us know what you think. Feel free to disagree, but if you do, you better be nice to Will.


2 comments:
I was fortunate enough to be present at Dr Hess' lecture during the AARC National Convention on this topic. He helped write the new VAE protocols. The objective was not to cut reimbursement more, it was to fix a broken system. Currently, if you ask any hospital what their VAP rate is they will say it is 0, or near 0. This is because they are relying on very subjective methods to classify VAP and there is incentive to classify it as something else even if they are doing things to treat it as VAP, such as giving antibiotics. The new system is much more objective and includes indicators for VILI as well as VAP.
It should also be pointed out that while VAE will be reported to the CDC for tracking purposes, there are no future plans for reporting VAE to Medicare/Medicaid for reimbursement purposes as of yet.
Thanks for the update.
Post a Comment